Sugarcoating mucus may ease its clearance in CF, other diseases
CF patients have lower levels of ST3Gal1, which helps make mucus less sticky
Written by |
Mucus-producing cells in people with cystic fibrosis (CF) have lower levels of ST3Gal1, an enzyme that sugarcoats mucus to make it less thick and sticky, but treatment with Trikafta can partly restore the enzyme and make mucus easier to clear away.
The findings, from a study led by researchers at the University of Alabama at Birmingham, suggest adding sialic acid, a type of sugar normally found in mucus, may be a way to treat CF and other diseases caused by abnormal mucus, according to a university news story. The study, “Reduced sialylation of airway mucin impairs mucus transport by altering the biophysical properties of mucin,” was published in Scientific Reports.
In CF, mutations in the gene that codes for the CFTR protein cause abnormally thick, sticky mucus to build up in the lungs and other organs. This can result in a range of symptoms, such as difficulty breathing and recurrent infections in the airways.
Mucus is rich in mucins, large proteins covered in sugar chains. Under healthy conditions, these chains often end with sialic acid, a negatively charged sugar that defines how mucus is structured and how well it’s cleared from the surface of organs.
Sugarcoating mucus
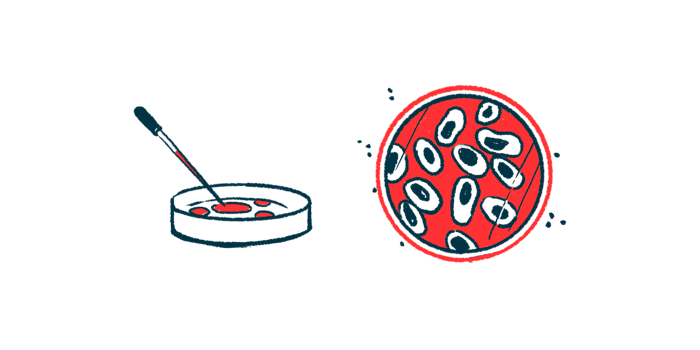
One of these mucins, MUC5B, is less charged in people with CF. How that changes mucus isn’t clear, leading the researchers to remove sialic acid from MUC5B in lab-grown human epithelial cells, a type of cell that releases mucus into the lining of organs.
Reducing the addition of sialic acid, a process called sialylation, resulted in slower-moving mucins in a gel, indicating less charge, and also led to more compact, entangled mucins, instead of them staying expanded. To see this, the researchers used electron microscopy, a technique that let them look at the detailed structure of MUC5B.
The results suggest reducing sialylation makes mucins more condensed, making mucus thicker and more difficult to clear away. In an experiment with a rat model, the flow of mucus along the windpipe was slowed down with treatment with an inhibitor of sialylation.
Compared to epithelial cells from healthy people, those from CF patients who carried two copies of F508del — the most common CF-causing mutation — had lower levels of ST3Gal1, an enzyme that adds sialic acid to mucins. When these cells were treated with Trikafta — a triple combination CFTR modulator approved for CF — ST3Gal1 increased, as did sialylation. This suggests restoring CFTR function may partially normalize mucus composition.
By showing that sialic acid is important for keeping mucus less thick and sticky, the study suggests sialylation could be a way to help clear out mucus in CF. It could also help with other diseases where mucus builds up, such as chronic obstructive pulmonary disease, or COPD.
“This study demonstrates the importance of mucin sialylation in mucus clearance and identifies decreased sialylation by ST3Gal1 as a possible therapeutic target in CF and potentially other muco-obstructive diseases,” the researchers wrote.