UCLA researcher wins grant to advance CF gene therapy delivery
Postdoctural scientist gets 2-year, $65K-per-year Elizabeth Nash Fellowship
Written by |

A researcher at the University of California, Los Angeles (UCLA) has been awarded the Elizabeth Nash Postdoctoral Fellowship to develop a targeted cystic fibrosis (CF) gene therapy delivery system, the university announced.
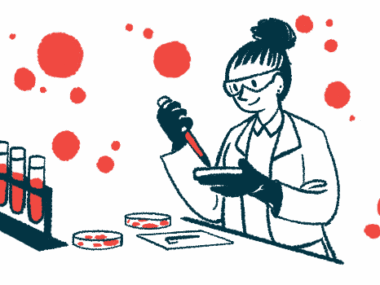
The two-year, $65,000-per-year fellowship, awarded annually by the Cystic Fibrosis Research Institute to support new and promising investigators, was granted to Ruby Sims, a postdoctoral scholar in pediatric hematology and oncology at the Broad Stem Cell Research Center and the Geffen School of Medicine at UCLA. Funded fellowship projects may be in basic, clinical, or translational research related to CF.
The goal of Sims’ project is “to create a targeted delivery system for gene editing and long-term curative treatments for cystic fibrosis patients,” the release states.
The project is titled “Designing a cystic fibrosis gene therapy nanocarrier platform to target and modify airway stem cell-derived ionocytes,” and will be conducted with Steven Jonas, MD, PhD, the principal investigator and a professor of pediatrics at the Geffen School of Medicine.
Sims also is the recipient of an Alex’s Lemonade Stand Young Investigator Award, according to the university. She plans to use that funding for a project in pediatric acute myeloid leukemia.
CF gene therapy delivery system project based on nanotechnologies
CF is caused by mutations in the CFTR gene that provides instructions for producing a protein of the same name. The CFTR protein is important for the production of mucus that lubricates body tissues. As a result of the mutations, CFTR is dysfunctional or missing, leading to a thick and sticky mucus that causes most disease symptoms.
Although treatments such as CFTR modulators have markedly increased CF patients’ quality of life and life expectancy, there are no gene therapies approved for the disease.
Pulmonary ionocytes, a rare cell type in the airways, have been found to have the highest level of CFTR gene activity, or expression, among airway cells. These cells have been successfully generated in the lab from stem cells derived from people with CF.
Researchers have been able to generate induced pluripotent stem cells — mature cells reprogrammed back to a stem cell-like state that can give rise to almost every cell type — from cells taken from patients. These cells were then used to create basal-like cells, precursor cells that can give rise to other airway cells.
In this project, the team will build upon nanotechnologies developed at the Jonas Lab to create a delivery system for a gene therapy targeting stem cell-derived ionocytes.
Previously developed nanotechnologies by Jonas and his collaborators included a nanoparticle/nanosubstrate-mediated system to deliver gene-editing technology. Gene editing can be used to modify or correct precise regions of DNA to treat serious diseases.
The ultimate goal is that based on nanotechnologies, the scientists can develop efficient delivery systems for CF gene therapies, potentially providing long-term curative treatments for the disease.