Medication-Blocking Mucus Barrier in Lungs Breached Using Nanoparticles
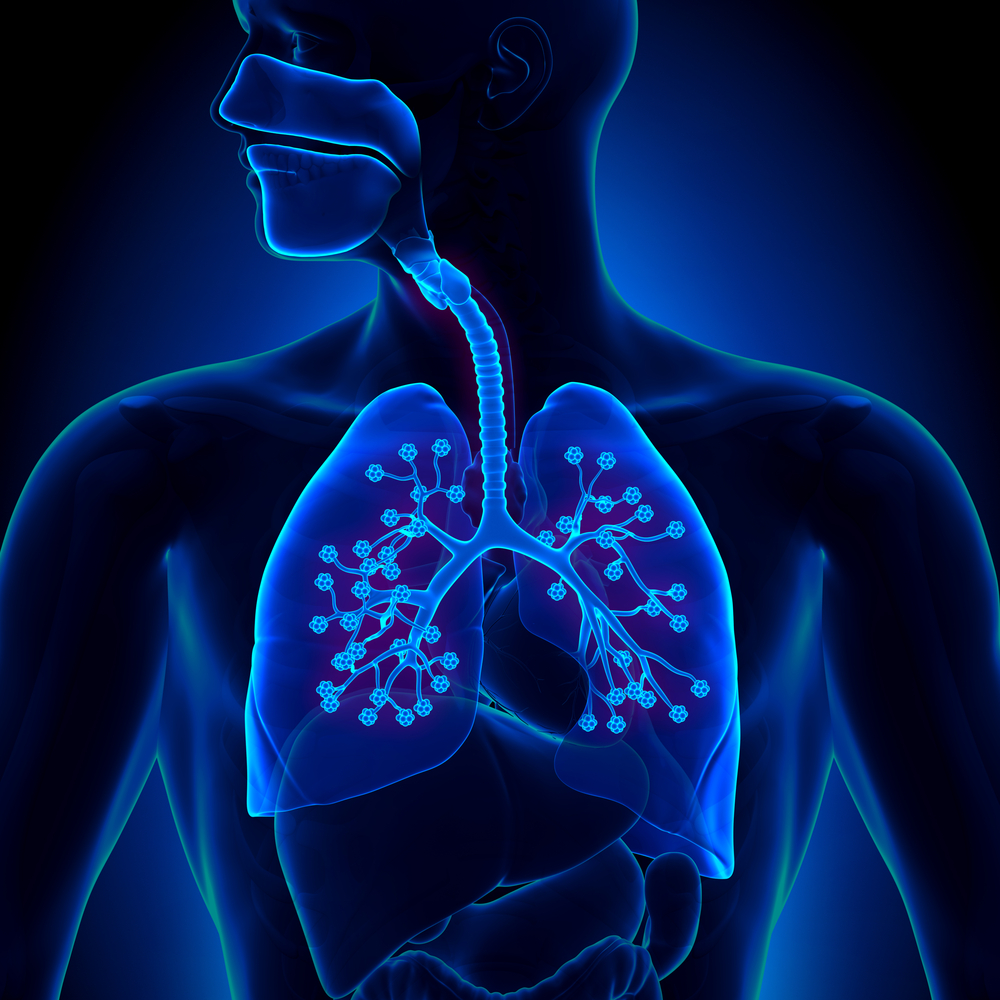
The first nanotechnology-enabled gene delivery system capable of efficiently penetrating the hard-to-breach mucus barrier shielding human airway and lung tissue may have been discovered with potential to one day develop an inhaled vehicle for delivery of targeted therapeutic genes that may be delivered directly to the lungs at levels sufficient to treat cystic fibrosis (CF), chronic obstructive pulmonary disease, asthma and other life-threatening lung diseases.
A DNA-loaded proof-of-concept nanoparticle that is able to pass through the lung mucus barrier has been designed by team of researchers at the Johns Hopkins University School of Medicine, Johns Hopkins University Department of Chemical and Biomolecular Engineering in Baltimore, Maryland, and the Federal University of Rio de Janeiro in Brazil.
“To our knowledge, this is the first biodegradable gene delivery system that efficiently penetrates the human airway mucus barrier of lung tissue,” says study lead author Jung Soo Suk, Ph.D., a biomedical engineer and faculty member at the Center for Nanomedicine at the Wilmer Eye Institute at Johns Hopkins.
A report on the work appeared in the Proceedings of the National Academy of Sciences on June 29, entitled “Highly compacted biodegradable DNA nanoparticles capable of overcoming the mucus barrier for inhaled lung gene therapy“ (Published online before print June 29, 2015, doi: 10.1073/pnas.1502281112
PNAS July 14, 2015 vol. 112 no. 28 8720-8725). The paper is coauthored by Panagiotis Mastorakosa, Adriana L. da Silva, Jane Chisholm, Eric Song, Won Kyu Choi, Michael P. Boyle, Marcelo M. Morales, Justin Hanes, and Jung Soo Suk, variously of the Center for Nanomedicine and Department of Ophthalmology at the Johns Hopkins University School of Medicine Wilmer Eye Institute in Baltimore, the Federal University of Rio de Janeiro’s Laboratory of Cellular and Molecular Physiology at the Carlos Chagas Filho Institute of Biophysics in Rio de Janeiro, the Johns Hopkins University Department of Chemical and Biomolecular Engineering, Center for Biotechnology Education, Krieger School of Arts and Sciences, and the Adult Cystic Fibrosis Program, Division of Pulmonary and Critical Care Medicine at Johns Hopkins University School of Medicine.
The coauthors note that therapeutically relevant lung gene therapy is yet to be achieved, but toward that goal they have introduced a highly translatable gene delivery platform for inhaled gene therapy based on state-of-the-art biodegradable polymers, poly(-amino esters). The researchers’ newly designed system is capable of overcoming challenging biological barriers, thereby providing robust transgene expression throughout the entire luminal surface of mouse lungs. Moreover, they report that provides markedly greater overall transgene expression in vivo compared with gold standard platforms, including a clinically tested system — the clinical relevance of which they say is further underscored by the technique’s excellent safety profile in addition to long-term and consistent transgene expression achieved following a single and repeated administrations, respectively.
The investigators observe that gene therapy has emerged as an alternative for treatment of diseases that stubbornly fail to conventional therapeutics, maintaining that synthetic nanoparticle-based gene delivery systems provide highly tunable platforms for delivery of therapeutic genes.
However, the inability to achieve sustained, high-level transgene expression in vivo presents a significant obstacle to be overcome, with the respiratory system, although readily accessible, remaining a challenging objective for scientists. The coauthors observe that effective gene therapy mandates colloidal stability in physiological fluids and the ability to overcome biological barriers found in the lung, so accordingly they formulated highly stable DNA nanoparticles based on state-of-the-art biodegradable polymers, poly(-amino esters) (PBAEs), possessing a dense corona of polyethylene glycol. The researchers found that these nanoparticles efficiently penetrated the nanoporous and highly adhesive human mucus gel layer that constitutes a primary barrier to reaching the underlying epithelium of lung tissue, and also discovered that these PBAE-based mucus-penetrating DNA nanoparticles (PBAE-MPPs) provided uniform and high-level transgene expression throughout the mouse lungs, superior to several gold standard gene delivery systems. PBAE-MPPs achieved robust transgene expression over at least 4 mo following a single administration, and their transfection efficiency was not attenuated by repeated administrations, underscoring their clinical relevance. Importantly, PBAE-MPPs demonstrated a favorable safety profile with no signs of toxicity following intratracheal administration observed.
The mucus barrier protects foreign materials and bacteria from entering and/or infecting lungs, and in healthy lungs, inhaled particle in the air are typically trapped in airway mucus to be subsequently swept away from the lungs via beating activities of cilia, or small, hairlike strands that line airway passages, and delivered to the stomach for degradation and elimination through the intestinal tract. “Unfortunately,” Dr. Suk notes in a Johns Hopkins release, “this essential protective mechanism also prevents many inhaled therapeutics, including gene-based medicine, from reaching their target.”
His team’s experiments with human airway mucus and small animals, Dr. Suk adds, were designed as a proof-of-concept study to demonstrate that by placing corrective or replacement genes or drugs inside a man-made biodegradable nanoparticle wrapper that patients inhale, the therapeutic agent(s) could penetrate the mucus barrier — a technique that could one day be used to treat serious lung disorders. Moreover, because a single dose might theoretically last for several months, patients would experience fewer side effects than are common to drugs that must be taken regularly over long intervals of time.
Dr. Suk says work with nanoparticles in his lab grew out of failed efforts to deliver treatments to people with lung diseases. CF patients for instance experience buildups of excess mucus caused by impaired ciliary beating that create ideal breeding grounds for chronic bacterial infection and inflammation. This pathogenic process not only worsens patients’ quality of life, it often puts them in life-threatening situations and also makes the airway mucus barrier even harder to overcome by inhaled therapeutic nanoparticles.
The researchers note that most existing CF drugs work to help clear infections but do nothing to solve the disease’s underlying issues, and a couple of recently approved drugs designed to target the underlying cause of CF require daily treatment for the patient’s entire lifetime and can benefit only a subpopulation of patients with specific types of mutations.
By contrast, this study, Dr. Suk points out, has demonstrated that delivery of normal copies of CF-related genes or corrective genes via mucus-penetrating DNA-loaded nanoparticles could mediate production of normal, functional proteins long term, and could eventually become an effective therapy for CF patients, regardless of mutation type.
 “To date, no one has been able to figure out how to efficiently deliver those genes to the lungs,” Dr. Suk observes, noting that experiments using deactivated viruses to carry them have proven inefficient and expensive, and could potentially lead to severe side effects. Moreover, the body could develop resistance to these virus-based delivery systems, rendering the delivery mechanism moot.
“To date, no one has been able to figure out how to efficiently deliver those genes to the lungs,” Dr. Suk observes, noting that experiments using deactivated viruses to carry them have proven inefficient and expensive, and could potentially lead to severe side effects. Moreover, the body could develop resistance to these virus-based delivery systems, rendering the delivery mechanism moot.
Alternatively, he says the while numerous nonviral, synthetic systems have been widely tested, previous research had shown that most of the nonviral, DNA-loaded nanoparticles possess positive charge that caused them to adhere to negatively charged biological environments, in this case the mucus covering the lung airways. In other words, conventional nanoparticles are too sticky to avoid unwanted off-target interactions distracting them from their journey toward target cells. Additionally, these particles tend to rapidly aggregate in physiological conditions, rendering them too large to penetrate the airway mucus barrier.
Accordingly, the team of investigators developed a simple method in which the nanoparticles were densely coated with the nonsticky polymer PEG which neutralized the charge and created a nonsticky exterior. They demonstrated that these  nanoparticles retained their sizes at a physiological environment and are capable of rapidly penetrating human airway mucus samples freshly collected from patients visiting the Johns Hopkins Adult Cystic Fibrosis Program directed by paper co-author Dr. Michael Boyle, who is currently Vice-Chair of the CF Foundations National CF Therapeutic Development Network and principal Investigator for the International Clinical Trials of VX-809 in F508del homoygotes, and whose lab’s research is focused on clinical trials for the development of new CF therapies.
nanoparticles retained their sizes at a physiological environment and are capable of rapidly penetrating human airway mucus samples freshly collected from patients visiting the Johns Hopkins Adult Cystic Fibrosis Program directed by paper co-author Dr. Michael Boyle, who is currently Vice-Chair of the CF Foundations National CF Therapeutic Development Network and principal Investigator for the International Clinical Trials of VX-809 in F508del homoygotes, and whose lab’s research is focused on clinical trials for the development of new CF therapies.
The research team also made the whole delivery system biodegradable so that it would not build up inside the body, and in order too test whether the system provides efficient gene transfer to the lungs of animals packed them with a gene that makes light-generating proteins once delivered into the target cells. Using mouse models they succeeded in demonstrating that inhaled delivery of genes via mucus-penetrating nanoparticles resulted in widespread production of the protein to levels superior to gold-standard, nonviral platforms, including a clinically tested system. In addition, they found that the treated lungs lit up for up to four months subsequent to a single dosing.
“With one dose, you can get gene expression i.e., production of therapeutic proteins for several months,” Dr. Suk says, adding that the nanoparticles did not appear to show any adverse effects, such as increased lung inflammation.
However, Dr.Suk and his team caution that more animal studies will be needed to confirm and refine their proof-of-concept study, and that treatment of human disorders with nanowrapped therapies remains years away.
The study was funded by the National Heart, Lung, and Blood Institute of the National Institutes of Health under grant numbers P01 HL51811 and R01HL127413 and the Cystic Fibrosis Foundation under grant numbers HANES07XX0 and HANES15G0.
Sources:
Johns Hopkins University School of Medicine
Proceedings of the National Academy of Sciences
Image Credits:
Johns Hopkins University School of Medicine