New Mouse Model May Lead to CF and COPD Therapies, Study Says
A mouse model that reproduces the human symptoms of cystic fibrosis (CF) and chronic obstructive pulmonary disease (COPD) gives scientists a new way to study, and perhaps develop treatments for, the diseases, according to new research.
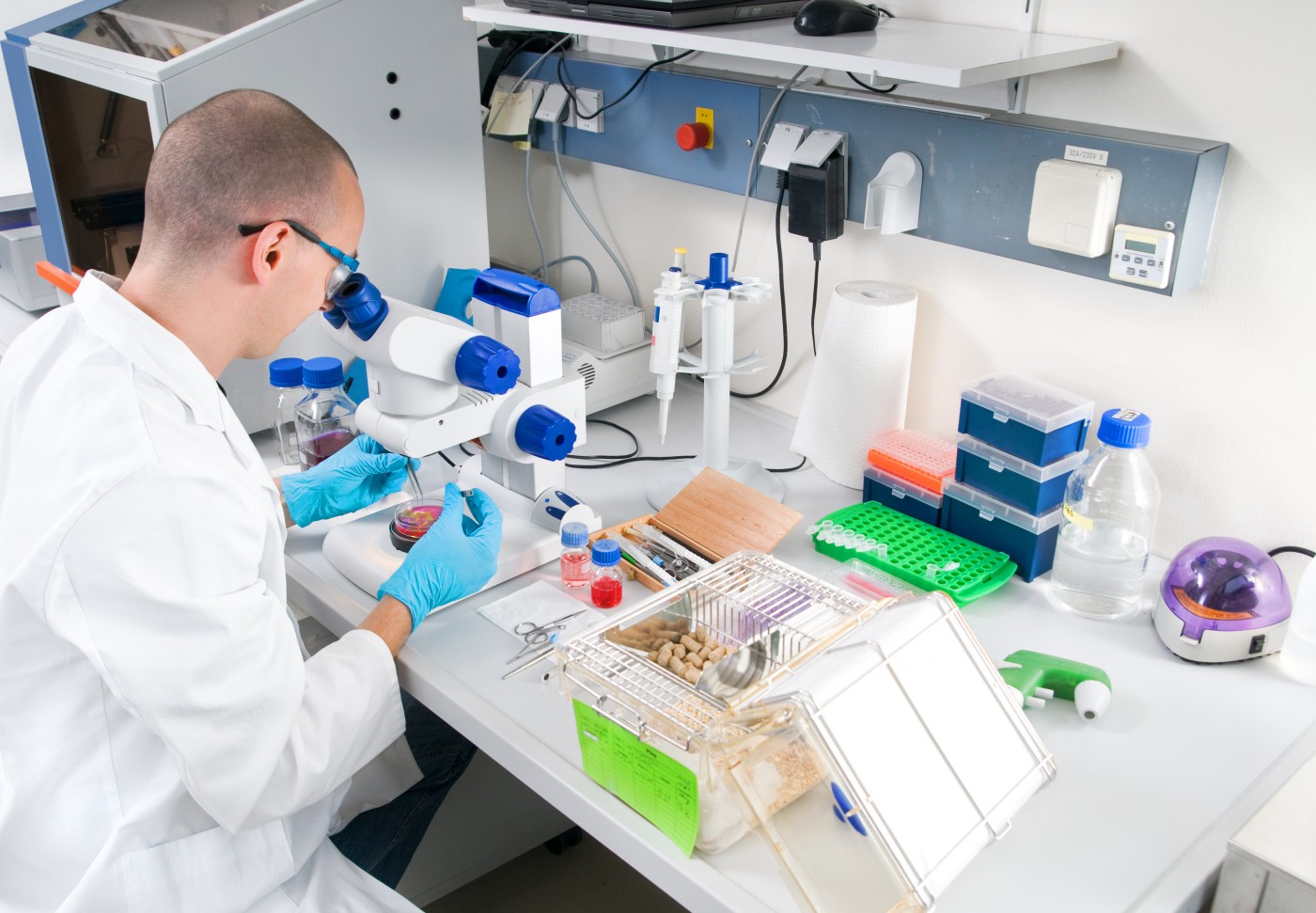
Researchers at Kumamoto University in Japan developed the model, then tested it to see how much it resembled the human versions of the diseases. The model shows alterations in two signaling pathways — oxidative stress and protease-antiprotease imbalance — that are similar to the alterations in human CF and COPD, they discovered.
The study, “Pharmacological and genetic reappraisals of protease and oxidative stress pathways in a mouse model of obstructive lung diseases,” was published in the journal Scientific Reports.
The model consists of mice whose genome was altered through genetic engineering to express — or promote — an epithelium-sodium channel (ENaC) in the lung’s pulmonary-epithelium cells. The channel regulates lungs’ water content and mucus production.
Researchers have done previous studies of the channel, but the transgenic — or genetically altered mice — used in the research had high death rates.
“Since previous mouse models have thus far only been produced by a limited number of studies, and had mortality rates that were quite high, we changed the genetic background of the ENaC-Tg mice using a ‘backcross’ method: a method that results in offspring that more closely resemble the parent genetically,” Tsuyoshi Shuto, an associate professor who headed the research team, said in a press release. “We then tested for specific molecules and pathways that lead to disease development in the mouse model.
The result, he said, was that the team “succeeded in establishing a new COPD/CF mouse model that faithfully reproduces the symptoms of the human diseases but with mortality significantly improved. Our model includes retention of mucus in the bronchus, reduction of lung function, pulmonary emphysema, and pulmonary inflammation.”
Researchers discovered that the new mouse model altered the expression of 272 genes in lung tissue.
Importantly, several of the genes are also responsible for increased expression in human CF and COPD. They include genes involved in oxidative stress — or lack of oxygen — and activation of protease, an enzyme that breaks down proteins and peptides.
“The ENaC protein activated in this animal model is also over-activated in the lungs of patients with cystic fibrosis (CF), which is an extremely frequent genetic disease in Europe and the United States,” Shuto said. “Development of this mouse model provides useful information not only for COPD/CF, but also for understanding other intractable pulmonary diseases and their drug treatment.”