Bacteria Boosts Anti-fungal Medicine’s Killing Power in CF Study
Co-infection with the bacterium Pseudomonas aeruginosa can increase the potency of therapies that kill Candida albicans, an infectious fungus, according to a new study.
The study, “Pseudomonas Synergizes with Fluconazole against Candida during Treatment of Polymicrobial Infection,” was published in Infection and Immunity.
Pseduomonas and Candida are both microorganisms that can cause infections in the lungs, particularly in people with underlying health conditions such as cystic fibrosis (CF). About three-quarters of CF patients have one infection or the other and sometimes both at the same time, which is generally tied to a more severe disease course.
Little is known about how co-occurring infections affect the response to treatment. A trio of scientists at the University of Maine conducted tests using fluconazole (FLC), an anti-fungal medication that is commonly used to manage Candida infections.
Infections with more than one microorganism “are challenging to treat not only because of the lack of understanding of how invading microorganisms interact but also because we don’t know how these interactions affect treatment efficacy,” Siham Hattab, the study’s lead author, said in a press release.
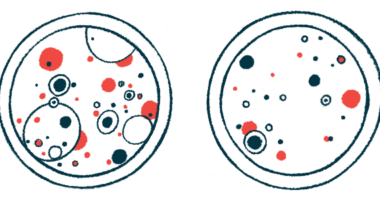
In lab dish experiments, the researchers used FLC to treat Candida fungi, either alone or in the presence of Pseudomonas. When Candida was grown with Pseudomonas in the absence of treatment, the bacteria had little to no effect on the fungus’ growth.
Treatment of Candida alone with FLC was fungistatic, but not fungicidal — that is, it stopped the fungus from growing, but did not kill it. However, when FLC treatment was given in the presence of Pseudomonas, the medication powerfully killed the fungus, reducing Candida counts by more than 1,000 times.
“We found that fungal-bacterial interactions can drive an unexpected enhancement in antifungal susceptibility during treatment of infection. Specifically, P. aeruginosa brings out a fungicidal activity of the normally fungistatic drug fluconazole against C. albicans,” the researchers wrote.
“The fungicidal effect of FLC during co-infection suggests that Pseudomonas blocks C. albicans tolerance to FLC, leading to death rather than persistence or slow growth during treatment,” they added.
The team then tested a zebrafish infection model. FLC treatment of fish that were co-infected with both Candida and Pseudomonas resulted in a statistically significant decrease in mortality. By contrast, treating fish only infected with Candida tended to reduce mortality, but the difference was not statistically significant.
“This indicates that FLC is more effective in treating C. albicans–P. aeruginosa co-infection than fungal mono-infection, suggesting that there is also bacterial-drug synergy in vivo [in living animals],” the researchers concluded.
Research showed this effect may be driven in part by the two microbes competing for iron, a nutrient that both Pseudomonas and Candida require to survive. Iron levels have been reported to be high in cystic fibrosis airways and involved in P. aeruginosa infections.
Supplementing the microorganisms with iron reduced, but did not eliminate, Pseudomonas and FLC’s synergistic anti-fungal effect, which also was reduced when Pseudomonas were engineered to lack iron-binding proteins called siderophores.
“While it is clear that P. aeruginosa has synergy with FLC against C. albicans in vitro [in lab dishes] and during co-infection, iron homeostasis is only one piece of the puzzle,” the researchers wrote.
They suggested that targeting iron-related biology could be a useful therapeutic strategy for these infections, but emphasized that more research into the specific mechanisms was needed.
“Our work demonstrates that polymicrobial interactions can indeed affect treatment efficacy and, most importantly, it highlights the importance of nutrient availability in the environment — such as iron in our study — and how it modulates treatment efficacy,” said Hattab, who conducted the research as part of her PhD training.