New molecules show promise against 2 common bacteria species
Staphylococcus aureus, Pseudomonas aeruginosa target of engineered molecules
Researchers have synthesized two new molecules that are able to kill Staphylococcus aureus and Pseudomonas aeruginosa — two species of bacteria that commonly cause lung infections in people with cystic fibrosis (CF).
These new molecules, known as synthetic nano-engineered antimicrobial polymers or SNAPs, showed synergistic bacteria-killing effects when combined with older antibiotics like penicillin, according to the study, “Combining SNAPs with antibiotics shows enhanced synergistic efficacy against S. aureus and P. aeruginosa biofilms,” which was published in the journal npj Biofilms and Microbiomes.
Bacterial lung infections are a frequent issue for many people with CF. These infections can be difficult to treat, and it’s becoming increasingly common for bacteria to evolve, resisting commonly used antibiotics.
SNAPs are a class of human-made molecules designed to mimic the activity of antimicrobial peptides (AMPs), which are naturally occurring small proteins that can kill bacteria. AMPs have been explored as potential antibacterial treatments, but the naturally occurring molecules can be toxic for human cells and usually aren’t stable in the human body, which has hindered their use. SNAPs aim to retain the bacteria-killing effects of AMPs without these issues.
g-D50 and a-T50 tested for bacteria-killing effects
Researchers in the U.K. engineered two new SNAPS, which they dubbed g-D50 and a-T50. After a series of tests to characterize the chemical properties of these new molecules, the scientists tested their bacteria-killing effect, both alone and when used in combination with older antibiotics.
Results suggested g-D50 could effectively kill S. aureus, and it had synergistic effects with beta-lactams (a class of antibiotics that includes penicillin and amoxicillin). Meanwhile, a-T50 could kill P. aeruginosa, and showed synergy with polymyxins (such as polymyxin B and colistin).
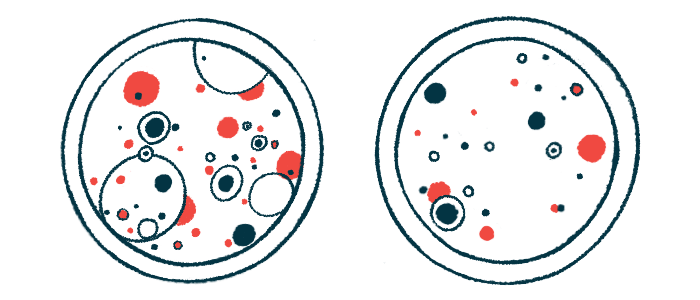
In a CF lung infection model derived from pigs, treatment with a-T50 on its own was not able to clear an established P. aeruginosa infection. However, when the SNAP was combined with colistin, there was a significant synergistic effect, acting to kill the bacteria and remove their biofilm, slimy layers of microorganisms that stick to wet surfaces and other bacteria.
“The combination of a-T50 and colistin showed a potent antibiofilm activity against P. aeruginosa biofilms in an ex vivo pig lung model of CF lung biofilm,” the researchers wrote. “The synergistic combination could reduce the doses of colistin used in clinics, reducing [toxic effects on human cells] while maintaining a potent antibiofilm activity.”
Further tests done in laboratory models showed g-D50 had the ability to prevent the formation of S. aureus biofilm, and this effect could synergize with penicillin treatment. The scientists concluded that “combinations of SNAPs with antibiotics show a potent synergistic effect to tackle biofilm infections in several advanced biofilm models.”