Broad analyses of lung microbiome could be useful for CF monitoring
Microbiota data may provide some additional insights in clinical practice
Written by |
The diversity and relative abundance of microbes in the lungs — or the lung microbiome — was generally stable over an eight-month period in people with cystic fibrosis (CF), regardless of whether they had experienced a pulmonary exacerbation, according to a recent study.
In the short term, using antibiotics to treat a pulmonary exacerbation — where lung symptoms acutely worsen — was linked to a decrease in overall bacterial diversity. Final statistical analyses indicated that only lung function during periods of clinical stability, but not microbial dynamics, was predictive of a pulmonary exacerbation.
“Complex microbiota data may provide some additional insights when used in combination with routine clinical measurements,” researchers wrote.
The study, “Longitudinal changes in the cystic fibrosis airway microbiota with time and treatment,” was published in the Journal of Cystic Fibrosis.
Lungs colonized by microbes, collectively known as the airway microbiome
The lungs are colonized by a wide variety of microbes, collectively known as the airway microbiome, most of which are not harmful to the human body. In CF, however, the accumulation of thick and sticky mucus in the lungs promotes an environment where harmful, infection-causing microbes predominate and bacterial diversity is diminished.
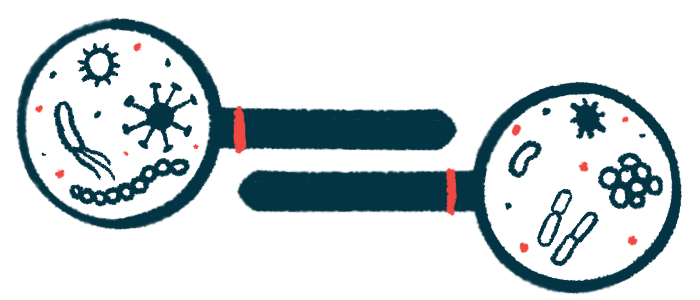
Samples of sputum mucus and saliva from the airways are routinely collected from CF patients and tested for known infection-causing bacteria, such as Pseudomonas aeruginosa. Although it is often assumed that an increased burden of these main culprits drives pulmonary exacerbations and lung function declines in CF, the airway microbiome is very complex, and it’s possible that changes in other types of microbes also contribute.
In the study, the researchers explored the possibility that a broader analysis of the entire airway microbiome, including the overall bacterial burden and diversity, might be useful for monitoring CF patients.
At least one sputum sample was collected from 149 CF patients seen at three CF clinics across Ireland and the U.S. Patients (44.6% female) had a mean age of 26.3. The study was conducted prior to the approval of CFTR modulator therapies, and thus no patients were using them.
First, the scientists looked at how the overall microbial community in the sputum changed over time for patients who had more than one sample collected (114 people).
Total bacterial density (amount of bacteria) did not change between patients’ first and last collected sputum samples, which were obtained on average about eight months apart and at times of clinical stability. Likewise, the relative abundance of detected types of bacteria and overall bacterial diversity was generally stable over time, as was lung function.
Decreases in bacterial diversity occur over many years in CF patients
This lack of change confirms reports that decreases in bacterial diversity occur over a much longer time frame — the span of many years — in CF patients, according to the researchers.
This microbial stability was also observed regardless of whether patients had experienced a pulmonary exacerbation and were treated with antibiotics during that time, “consistent with a lower airway ecosystem that is resilient and rapidly resets after intense antibiotic pressure,” the researchers wrote.
When patients were stratified by whether they had a higher or lower P. aeruginosa abundance in their first collected sample, only those with a higher P. aeruginosa burden showed changes in bacterial diversity over time.
A total of 62 patients were given acute antibiotic treatments for a pulmonary exacerbation.
No significant differences were observed in overall bacterial density before and after the exacerbation, with samples collected about 17 days apart. On the other hand, overall bacterial diversity was significantly reduced following antibiotic treatment, particularly in patients with greater lung function improvements and who had a lower P. aeruginosa burden.
Finally, the scientists aimed to identify possible predictors of future pulmonary exacerbations by comparing clinical features between patients who did and did not experience one during the study.
Lung function found to significantly predict pulmonary exacerbation risk
Higher lung function, increased body mass index (a measure of body fat), and greater overall bacterial diversity in sputum samples was associated with lower odds of pulmonary exacerbations, while long-term use of certain antibiotics was linked to higher odds. However, in final statistical analyses, only lung function was found to significantly predict pulmonary exacerbation risk.
Altogether, the researchers believe the findings emphasize the potential utility of broad microbiome analyses for monitoring CF patients and their responses to treatment.
They noted, however, that “analyses of the sputum microbiota requires considerable expense and expertise.” As such, larger clinical trials are still needed to evaluate how feasible the approach is for use in clinical practice.
“Furthermore, whether microbiota associated metrics could be used to help inform selection of antibiotics, guide duration of therapy or identify those who do not respond to treatments are of interest and require further investigation,” the team concluded.