#ECFS2018 – Phase 2 Trial Supporting SPX-101 as Treatment for All with CF, Spyryx CMO Says
Written by |
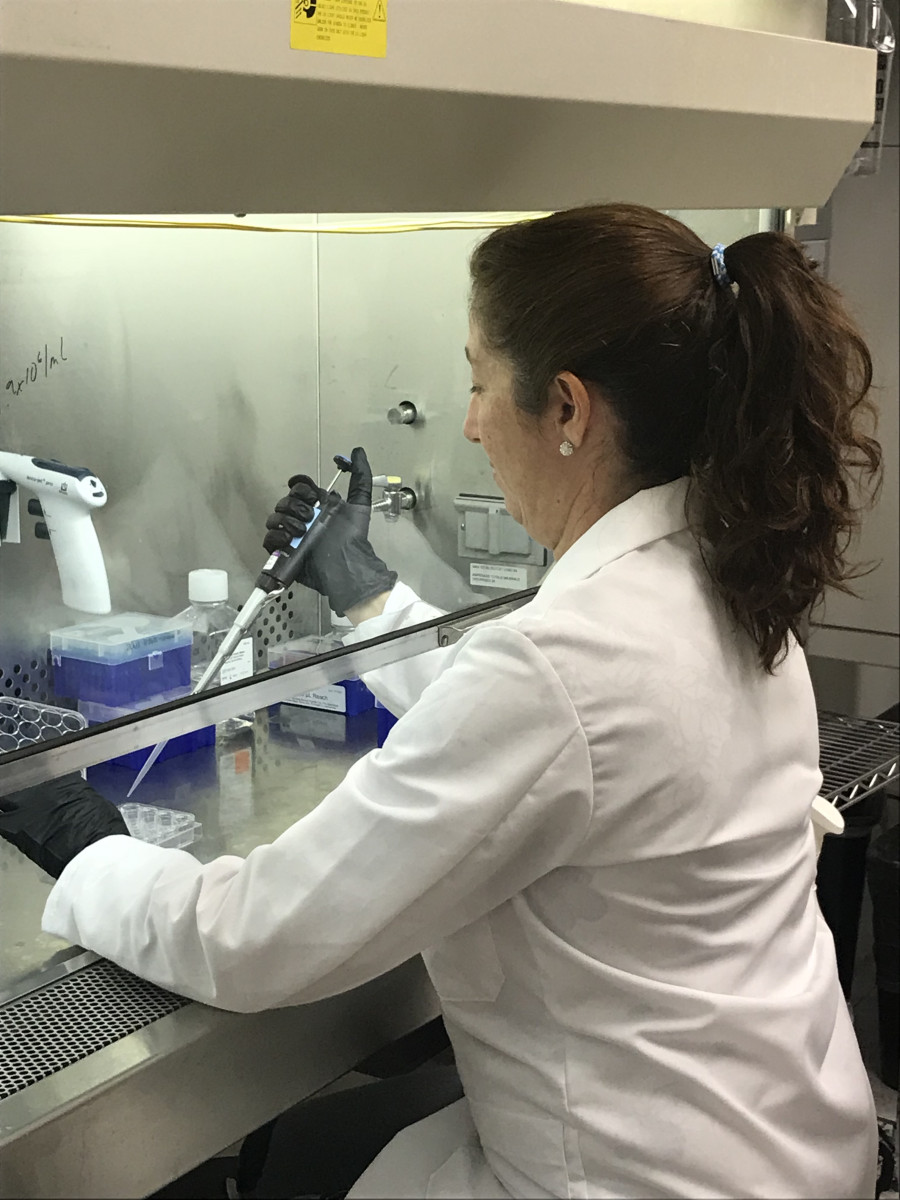
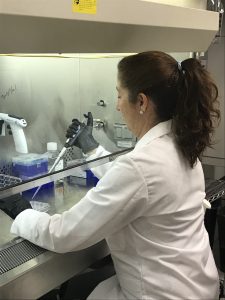
Juliana Sesma, PhD, works in the Spyryx lab in Durham, N.C. (Photo courtesy of Spyryx)
SPX-101, designed to help clear mucus from the lungs of people with cystic fibrosis, has the potential to treat all CF patients — regardless of disease-causing mutations.
The experimental peptide, which blocks the overactive sodium channels that line CF lung cells so more fluids are retained on airway surfaces to hydrate mucus, was developed by Spyryx Biosciences. Isabelle Fajac, president of the European Cystic Fibrosis Society, presented results of an ongoing Phase 2 clinical trial of SPX-101 during the 41st European Cystic Fibrosis Conference (ECFS) in Belgrade, Serbia.
Ahead of Fajac’s presentation, British pulmonologist Alistair Wheeler — the chief medical officer of Spyryx — spoke at length with Cystic Fibrosis News Today about SPX-101 and why he thinks his company can make a difference in the lives of CF patients.
“Our work comes out of some discoveries Dr. [Robert] Tarran made at the University of North Carolina-Chapel Hill about five years ago,” he said, referring to the UNC researcher’s work on the role of the epithelial sodium channel (ENaC) in keeping airways properly hydrated.
A result of that work — SPX-101 — may improve on earlier inhibitors in two crucial ways.
“Previous ENaC inhibitors were limited by life-threatening increases in potassium, the sort that can stop your heart without warning,” Wheeler said. “In all of our studies, at any dose, in healthy subjects and in those with cystic fibrosis, we have not seen a dose-limiting effect on serum potassium.”
ENaC inhibitors are known to promote potassium retention by the kidneys, raising blood potassium levels (a condition known as hyperkalemia) and risking kidney failure.
They also generally have a very short duration of action — a short lifespan, if you will.
“They rehydrate the airway, and then the additional water washes them away. It’s like turning on the tap. So our approach has been to internalize the channel into the cell, so even if the peptide gets washed away, it still has activity,” Wheeler said.
“Our peptide doesn’t get into the system to the same extent and is cleared more quickly,” he added, pinpointing those two ways.
CFTR and ENaC ‘work in parallel’
Fajac’s oral presentation, “A Double-Blind, Placebo-Controlled, Randomized Study of SPX-101, a Novel Peptide Modulator of ENaC Cell Surface Density in Adults With Cystic Fibrosis,” described the most recent results of the HOPE-1 trial (NCT03229252), which is evaluating the effectiveness and safety of SPX-101.
The data covers 40 patients (of 45 dosed in a first group) randomly given either 60 mg or 120 mg of SPX-101, or a placebo, twice a day for 28 days via the portable eFlow nebulizer. All had a forced expiratory volume in 1 second (FEV1; a measure of lung function) of 40 to 80 percent.
FEV1 increased by 5.19 percent compared to placebo in the overall population treated at 120 mg, meaning it “marginally missed” showing benefits of statistical significance. But in high-dose patients with better lung function — above 55 percent — SPX-101 showed an 8.3 percent improvement in FEV1 at day 28, a change that’s statistically significant.
“A 5 percent improvement is meaningful. Clearly, we would like it to be as good as it can be,” Wheeler said. But “it was important to note that in the mild and moderate [FEV1] population, we saw a better response at about 8 percent.”
In contrast, the FEV1 change among those treated at 60 mg twice daily compared to placebo was 3.08. A next group of patients will be tested at the high dose only, Wheeler said.
ENaC and CFTR — which stands for cystic fibrosis transmembrane conductance regulator — work in parallel.
“CFTR adds fluid to the airway and hence hydrates mucus. ENaC removes fluid and dehydrates mucus. Hence, we want to restore CFTR function and inhibit ENaC function,” he said. “In the best case, we would do both and therefore patients could certainly benefit from both.”
In other words, SPX-101’s use in combination with Vertex’s CFTR modulators likely “would be beneficial,” Wheeler said, adding his company has preclinical data supporting such use. But that was not the intent of this exploratory Phase 2 study.
Europe, Canada focus of HOPE-1
Wheeler, who came to the United States in 1991, received his medical training at Royal London Hospital and has had a 30-year career in the pharmaceutical industry, working for Glaxo and other multinationals. Spyryx, which employs eight people at an office park in Durham, North Carolina, spent two years getting SPX-101 through preclinical and Phase 1 and 2 testing; the current trial began in August 2017.
Non-U.S. sites were favored because Spyryx wanted to see what SPX-101 could do without a disease-modifying therapy.
“As a first patient study, we wanted a clear definitive answer as to whether this first cohort justified further development,” Wheeler said. “We were very keen to look at a population who were not using CFTR modulators, and the sad reality is that CFTR modulators are widely available in the United States, but not in Europe or Canada.”
HOPE-1, which is still enrolling participants, tested its first group at sites in Canada, France, Portugal, and the United Kingdom. The next phase will include Italy and possibly Australia. Likely, another 45 or so patients will be recruited.
SPX-101 took five to 10 minutes to dose, depending on the exact dosage given in the trial, but “about a five-minute administration” is the goal.
Because it’s formulated in normal saline, sodium chloride, it’s not overly salty, and the peptide itself is tasteless.
“In placebo-controlled studies, healthy volunteers could not tell any difference between the active and the placebo. It’s got a slightly salty taste, but it doesn’t have the negative attributes of hypertonic saline,” Wheeler said.
Treatment was safe and well-tolerated, with the most common side effects reported to be cough and increased sputum production.
“It sounds strange to say that’s an adverse effect, because that’s actually what we’re trying to do,” he said. “But if patients have a new experience, they’re required to report that, and the sites must report that as an adverse event. So, we had some cough and sputum, particularly around the time they [patients] were nebulized.”
In general, 65 to 70 percent of patients in all three groups — 60 mg, 120 mg and placebo — reported adverse events, which Wheeler said is about normal.
Four patients, three among those treated at 120 mg and one placebo patient, “deteriorated” during the study due to CF exacerbations or increased breathlessness, and chose not to continue. The fourth, also in the high-dose group, made the same decision after experiencing an increase in heart rate, Wheeler said.
Spyryx hopes to eventually test SPX-101 in children and adolescents, but such trials await further results.
“Conventionally, we don’t look at patients below 18 until we have established efficacy in adults,” he said. “The next phase of younger development will be adolescents aged 12 to 18. After adolescents, we would get down to ages 2 to 5. We need to complete HOPE-1 before we would begin younger studies.”
Work with a second HOPE-1 patient group should finish within one year.
“This [first] cohort was really exploratory. We were looking for the scientific justification to continue and expand the development of SPX-101,” he said. “The next cohort will be an extension of cohort 1, so we better understand the true benefits and variability within the patient population.”
An all-inclusive treatment
SPX-101 has the potential to be a “massively important” new therapy because it can help all CF patients, regardless of their specific mutation, Wheeler said.
“We know that the triple-therapy modulators will cover 90 percent of the population, but there’s still 10 percent — which is a lot of people — who won’t have any CFTR modulator,” he said. “In the medium- to long-term future, perhaps as long as 10 years, the approaches for those patients are really CRISPR and gene editing approaches, which are much further behind.”
Airway obstruction and structural damage to the lung, and not a given mutation, most likely determines the degree of SPX-101’s benefit in preventing ENaC channels from absorbing too much sodium. That absorption turns mucus thick and sticky, affecting breathing and raising the risk of lung infections.
Spyryx is limited by its preclinical work to 28 days’ exposure — setting the trial’s treatment duration — but that’s “an adequate period to show improvement with this type of agent,” Wheeler said. Once the company has additional data in hand, it may invite current patients back, and intended Phase 3 studies will certainly include longer treatment times.
For now, he said, there’s no need to go beyond 28 days.
Future clinical trials will also include patients on CFTR modulators in the U.S. and elsewhere.
Wheeler’s sure there is a place for SPX-101 alongside standard therapy.
“The reality is that every adult with cystic fibrosis has very substantial lung damage, with or without a transplant — and certainly without transplant. They are going to continue to need symptomatic and supportive therapy, and antibiotics and agents for mucus clearance.”
That need, and the people who suffer because of it, are key, he said.
“I’ve worked in other respiratory indications — asthma, COPD — and in a lot of cardiovascular indications,” but “I have never seen such unified passion to help patients as I have in cystic fibrosis,” Wheeler said. “And that’s true in the clinical centers, it’s true with the regulators, and it’s true in the biotech industry. There really is an extraordinary passion, patients first.”