CF Patients with Uncommon Lung Bacteria at Initial Risk of Exacerbations
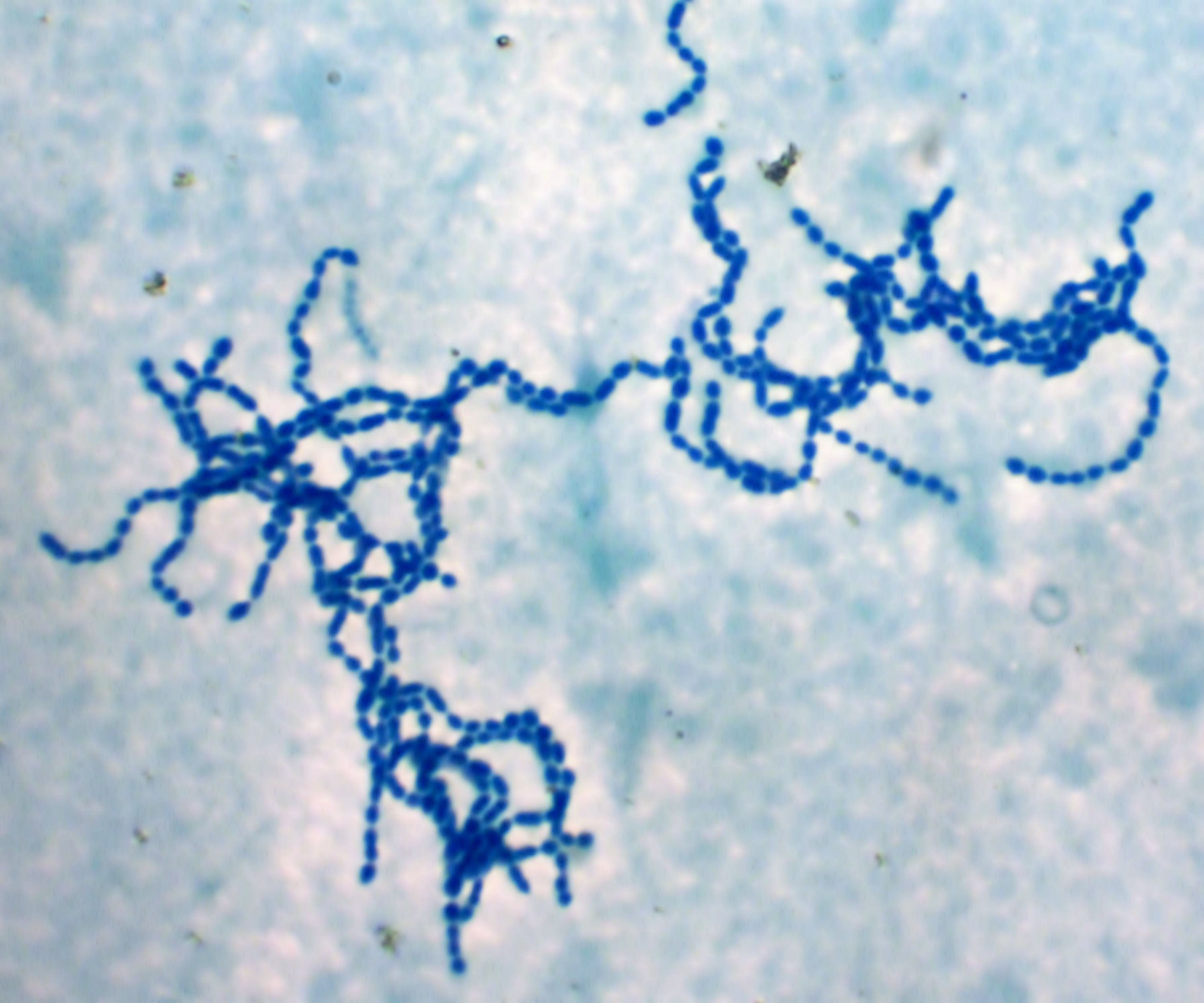
A recent study reported that the presence of transient Group A streptococcus (GAS) in patients with cystic fibrosis (CF) increases the risk of pulmonary exacerbations. The study, “Clinical implications and characterization of Group A Streptoccoccus infections in adults with cystic fibrosis,” was published in the journal BMC Pulmonary Medicine.
GAS infections are uncommon in CF, but can contribute to potentially dangerous community-acquired pneumonia. Non-classical pathogens infecting the lower airways of CF patients are also increasingly being reported.
To investigate the pattern and clinical impact of GAS infections in CF patients, a research team led by Kate Skolnik from the University of Calgary, Canada, analyzed biobank samples of 15 adults with CF where GAS was found to be the dominating microorganism. The biobank stored bacterial isolates from sputum samples that had been collected at clinical visits.
The team analyzed patient data ranging from two years before the bacteria were isolated to two years after detection. Patient demographics and worsening states, both medical and pulmonary, were evaluated. The primary outcome was worsening pulmonary symptoms at the time of GAS detection. The team also looked at changes in lung function and frequency of exacerbations after bacterial isolation.
The researchers noticed that almost half of the patients (47 percent) experienced pulmonary exacerbation at the time of GAS isolation. Half of these recorded events were classified as severe, and an exacerbation event was more likely when GAS was the dominant species isolated.
Following GAS isolation, the frequency of exacerbations was similar in GAS-infected and other patients. GAS infection also did not affect lung function decline in the study sample.
The researchers also tested if the bacteria were sensitive to commonly used antibiotics. They noticed that GAS was susceptible to anti-streptococcal antibiotics and anti-pseudomonal antibiotics often used in CF, with the exception of azithromycin.
The study reported that none of the patients developed chronic airways infection or other complications such as bacteremia, necrotizing pneumonia, or empyema following GAS infection. The authors concluded that transient GAS infections do not lead to chronic infections or altered long-term outcomes in CF patients exposed to the bacteria.







