Common Environmental Fungus Can Worsen Lung Function in CF Children
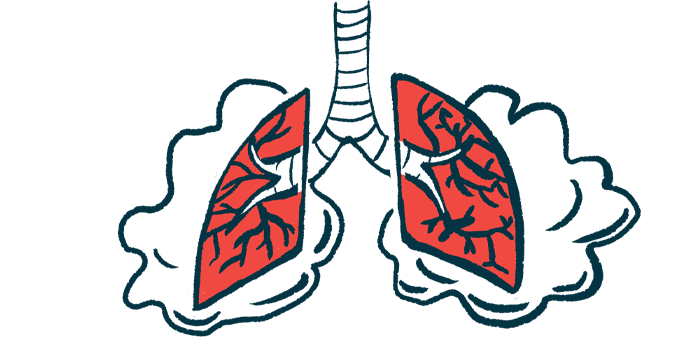
A fungus called Aspergillus fumigatus can significantly affect lung function and structure, as well as increase the number of pulmonary exacerbations — episodes of a sudden worsening of respiratory symptoms — in children with cystic fibrosis (CF), a study suggests.
The findings shed light on the need for early diagnosis to prevent serious and potentially irreversible lung damage, researchers say.
The study, “Clinical Impact of Aspergillus fumigatus in Children with Cystic Fibrosis,” was published in the journal Microorganisms.
A. fumigatus is commonly found indoors, as well as in water and soil. Although people inhale its spores daily without becoming sick, in patients with CF the fungus can chronically colonize the lungs and trigger inflammation in the airways.
Depending on the strength of a person’s immune system, and other factors, infection with A. fumigatus can promote hypersensitization (exaggerated response) to the fungus, Aspergillus bronchitis — infection of the bronchi, the main airways of the lungs — or allergic bronchopulmonary aspergillosis (ABPA), an allergic reaction to the fungus that may permanently damage the lungs.
Studies have shown that up to 50% of adult patients with CF test positive for A. fumigatus. However, the incidence of this fungus among children with CF has not been clarified. Additionally, how A. fumigatus impacts lung function and the health of young CF patients still needs further investigation.
Therefore, researchers at the University of Parma in Italy reviewed medical records from 2018 to 2020 to identify children with CF, ages 6 to 18 years. Blood tests were obtained annually, and samples of sputum or throat swabs were collected four times a year. Lung function was also assessed four times per year.
A total of 38 patients regularly seen at the Parma Cystic Fibrosis Regional Centre were ultimately included in the study. They ranged in age from 6 to 18, and 23 were boys.
The patients were classified as having ABPA, Aspergillus bronchitis, or being sensitized to A. fumigatus based on specific criteria, which included the total levels of immunoglobulin E (IgE, a type of antibody); the presence of Aspergillus-specific IgE; and chest X-rays suggestive for ABPA. Notably, chronic Aspergillus bronchitis was diagnosed when Aspergillus-specific antibodies were identified along with clinical deterioration, but no other criteria of ABPA were present.
While 21 patients showed no signs of A. fumigatus, eight (21%) had A. fumigatus sensitization, seven (18.4%) had ABPA, and one (2.6%) was diagnosed with Aspergillus bronchitis. One child (2.6%) had A. fumigatus colonizations detected in the sputum.
Patients with ABPA had lower body mass index (BMI), a measure of body fat based on weight-to-height ratio, and lower lung function, as measured by forced expiratory volume in one second (FEV1), compared to those without ABPA. Children with ABPA also had a significantly higher mean number of exacerbations (4.43 vs. 1.74 in the remaining patients) in the previous year.
FEV1 declined by nearly 7% over three years in all patients enrolled in the study, with the greatest decline in lung function being observed in those with ABPA.
Compared to the other groups, patients with ABPA were more likely to have pancreatic insufficiency, a common complication of CF.
Those with ABPA were also more likely to use long-term inhaled antibiotics (tobramycin, colistin, or levofloxacin), oral azithromycin, and inhaled steroids.
Chest CT scans were assessed using the Bhalla scoring system which quantifies structural lung abnormalities. Lower scores indicate more severe structural lung changes. The findings showed that the ABPA group and sensitized children had more abnormalities in lung structure than patients without A. fumigatus (Bhalla score of 14 for ABPA patients, 17.1 for those with A. fumigatus sensitization, and 22 for children with no signs of A. fumigatus).
“This study showed that Af [A. fumigatus] played a pivotal role in pediatric patients with CF and that ABPA and Af sensitization had a relevant clinical impact in terms of exacerbations and lung structural damage,” the researchers wrote.
“These findings highlight that annual screening for total serum IgE levels and Aspergillus-specific IgE levels is essential to intercept the onset of Aspergillus sensitization and/or signs of ABPA,” they added.