Neutrophils are associated with better lung function in CF: Study
Study shows how immune system is affected by the disease, researchers said
Certain neutrophils, a type of immune cell that’s released quickly into the bloodstream to help fight off infections, appear to be linked to better lung function in some people with cystic fibrosis (CF), a study finds.
The presence or abundance in the blood of certain other immune cells and their proteins may vary depending on which types of beneficial and harmful bacteria or fungi are in the lungs, the researchers said.
“Our work highlights how the overall immune system is affected in [people with CF],” they wrote in “Widespread alterations in systemic immune profile are linked to lung function heterogeneity and airway microbes in cystic fibrosis,” which was published in the Journal of Cystic Fibrosis.
The researchers said their findings may offer a starting point for identifying new biomarkers and treatment targets for CF, which nearly always affects the lungs, leading to trouble breathing and long-lasting infections, but can manifest uniquely in each patient. Why this happens is unclear, but it may be because of flaws in the immune response.
To capture a detailed picture of the immune profile that marks CF, researchers in Denmark collected samples of blood and sputum, or phlegm, from 28 people with the disease, ages 12-61, and a similar-aged group of healthy people.
Measuring immune cells in CF
Most patients (89.3%) had long-lasting infections caused by Pseudomonas aeruginosa bacteria and all but one had pancreatic insufficiency, which occurs when thick mucus prevents the pancreas from releasing enough digestive enzymes.
Most were on CFTR modulators, a type of treatment that address the root cause of CF. The most frequently prescribed was Symkevi (ivacaftor/tezacaftor; Symdeko in the U.S.), followed by Kaftrio (ivacaftor/tezacaftor/elexacaftor; Trikafta in the U.S.), Orkambi (ivacaftor/lumacaftor), and Kalydeco (ivacaftor).
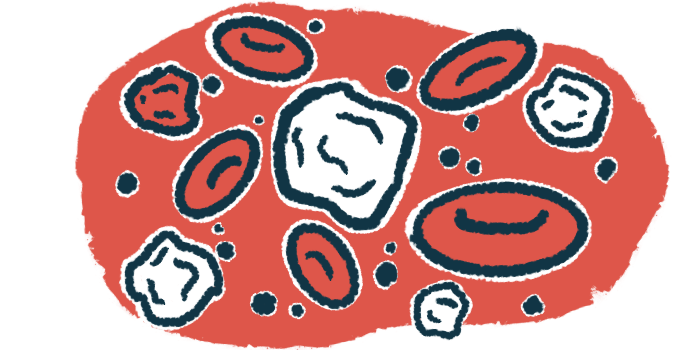
The researchers measured the totals of 82 different types of immune cells in the blood and found that people with CF had an immune cell pattern that clustered differently than the healthy people. Both parts of the immune system, the first line of defense, or innate, and the adaptive, that is, the targeted defense, contributed to that pattern.
People with CF had almost twice as many neutrophils, which are the immune cells that travel toward infections to ingest bacteria or release enzymes that destroy them.
Neutrophils of people with CF had 1.5 times more CD35, CD64, and CD69 — proteins that are markers of activation — than healthy people. CD11b, which affects cell adhesion and migration, was 1.5 times more abundant on immature neutrophils of CF patients. PD-L1, a protein that helps tune the immune response to prevent overactivity, was 13 times more abundant on neutrophils of people with CF over healthy people.
In contrast, there were fewer monocytes, an immune cell that’s reported to be faulty in CF. Subsets of dendritic cells, which help start and boost the immune response, were lower in CF patients, as were CD4-positive T-cells, which help direct the immune response.
Like neutrophils, however, both circulating monocytes and T-cells had a more active profile in people with CF than healthy people. B-cells, which together with T-cells form the adaptive immune system, also appeared not to be operating normally in CF.
Certain neutrophils and lung function
Based on the relative abundance of their immune cells, people with CF were divided into two groups — C1 (15 patients) and C2 (13 patients). C1 patients had significantly better lung function than C2, as seen by a higher percent predicted forced expiratory volume in one second (73% vs. 41%).
C1 patients had higher numbers of cells of both the innate and adaptive immune systems, including memory B-cells, which can quickly produce antibodies when they reencounter their targets, “suggesting an overall increase in cells involved in the protective B-cell response in C1,” the researchers wrote.
While higher numbers of mature neutrophils were linked to worse lung function, having a greater proportion of neutrophils with the CD35 and CD49 markers on their surface was linked to better lung function.
Sputum samples from 26 patients revealed a complex mix of bacteria and fungi. The collection of all microorganisms in the lungs was linked to how well they were working, but not with the overall immune cell profile.
The presence of harmful microorganisms like those of the Mycobacterium, Staphylococcus, and Aspergillus genera, but not Pseudomonas bacteria, were linked to lower numbers of T-cells and B-cells, whereas beneficial bacteria were linked to higher numbers of those immune cells.
The findings suggest the balance between harmful and beneficial bacteria or other microorganisms in the lungs may change the track of the immune response. “The coexistence of various members of microbial communities may influence the immune response in CF,” the researchers wrote.
An immune system that’s overactive and out of control, along with the presence of specific microorganisms in the lungs, may contribute to the unique ways the disease is experienced. Any immunomodulatory approach “should acknowledge the complex interactions” with the collection of microorganisms, called the microbiome, the researchers said.