Trikafta boosts production of immature CFTR protein, study finds
Findings may shed light on wide variability in response rates in CF patients
Trikafta increased the production of the faulty CFTR protein in cystic fibrosis (CF) patients, but it remained in an immature state, a study suggests.
These findings may shed light on the wide variability in response rates in CF patients and caution that immature CFTR protein may prevent sustained benefit from Trikafta treatment, researchers note.
The study, “Changes in cystic fibrosis transmembrane conductance regulator protein expression prior to and during elexacaftor-tezacaftor-ivacaftor therapy,” was published in the journal Frontiers in Pharmacology.
Trikafta is CFTR modulator containing three medicines
CF is caused by mutations that impair the function or production of the CFTR protein. Trikafta is a CFTR modulator therapy containing three medicines — elexacaftor, tezacaftor, and ivacaftor — that help improve CFTR protein production and function in patients with at least one F508del mutation, the most common CF-causing genetic defect, or another responsive mutation.
Both elexacaftor and tezacaftor work as correctors that help the faulty CFTR protein fold correctly, allowing its transport to the cell membrane instead of being degraded. Ivacaftor is known as a potentiator that supports CFTR protein function.
In clinical trials, Trikafta treatment eased many signs and symptoms of CF, improving lung function and nutritional status, among other benefits. However, the molecular consequences of Trikafta treatment on CFTR protein production have yet to be directly examined in CF patients.
Such data may help highlight mechanisms behind the wide variability in clinical responses and support long-term efficacy studies of Trikafta, noted researchers at the Hannover Medical School, in Germany.
The study included 15 female and six male CF patients ages 12 to 44 years. Six participants carried two F508del mutations (one from each parent), and 15 had mixed mutations: one F508del mutation and a second minimal function CFTR mutation.
Our results might provide a basis to understand different degrees in response and different long-term outcomes of [Trikafta] treatment.
Almost all participants had yet to be treated with Trikafta at the study’s start, except for the oldest patient who had previously received Symdeko, a tezacaftor/ivacaftor combination therapy.
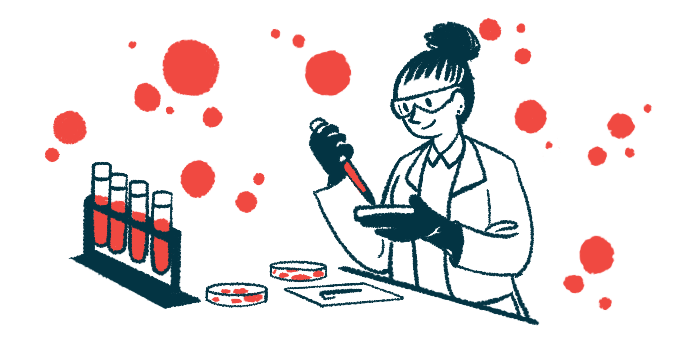
Tissue samples were collected from patients, as well as one non-CF healthy control, by a painless rectal suction biopsy and analyzed alongside commonly used lung and intestinal reference samples.
Consistent with clinical trials, Trikafta improved lung function and body mass index (a measure of body fat) and decreased the levels of sweat chloride, a biomarker for CF, in most participants.
In all samples except for CF biopsies, the analysis revealed two forms of CFTR protein, including a larger, fully mature form that is glycosylated — a process of attaching sugar molecules to proteins to help them fold properly and/or maintain stability.
CF patient samples also had the smaller form seen in non-CF samples but also a unique, partially glycosylated form here designated as CFTR C-star. Across all patient samples before Trikafta, 20 out of 21 had this CFTR C-star form and no detectable mature CFTR protein.
Immature CFTR protein levels higher in most patients after Trikafta treatment
After eight to 16 weeks of Trikafta, the signal for CFTR C-star was at least twofold higher than before treatment in eight out of 12 patients. However, in two of these samples, CFTR C-star dropped by about half after treatment, with the most substantial decline in CFTR C-star seen in one patient who carried one F508del mutation and one N1303K mutation.
Overall, CFTR C-star was higher in those with two F508del mutations compared to patients with mixed mutations. Four out of five F508del double carriers showed an increase in CFTR C-star of at least 300%. Five out of seven of those with mixed mutations also saw an increase but to a lesser extent. A drop in CFTR C-star after treatment was only seen in mixed mutation samples.
Despite the increase in CFTR C-star after treatment, it never became a fully mature CFTR protein, suggesting incomplete glycosylation after protein production. The researchers concluded CFTR C-star was the “status quo” form of F508del CFTR protein in CF patients.
“Our results might provide a basis to understand different degrees in response and different long-term outcomes of [Trikafta] treatment,” the team wrote. “They caution that the lower amounts or immature glycosylation of the [CFTR C-star form] might prevent long-term, sustained benefit of [Trikafta].”