Discovered Bacteria ‘Wars’ May Lead to New Antimicrobial Treatments for CF, Study Suggests
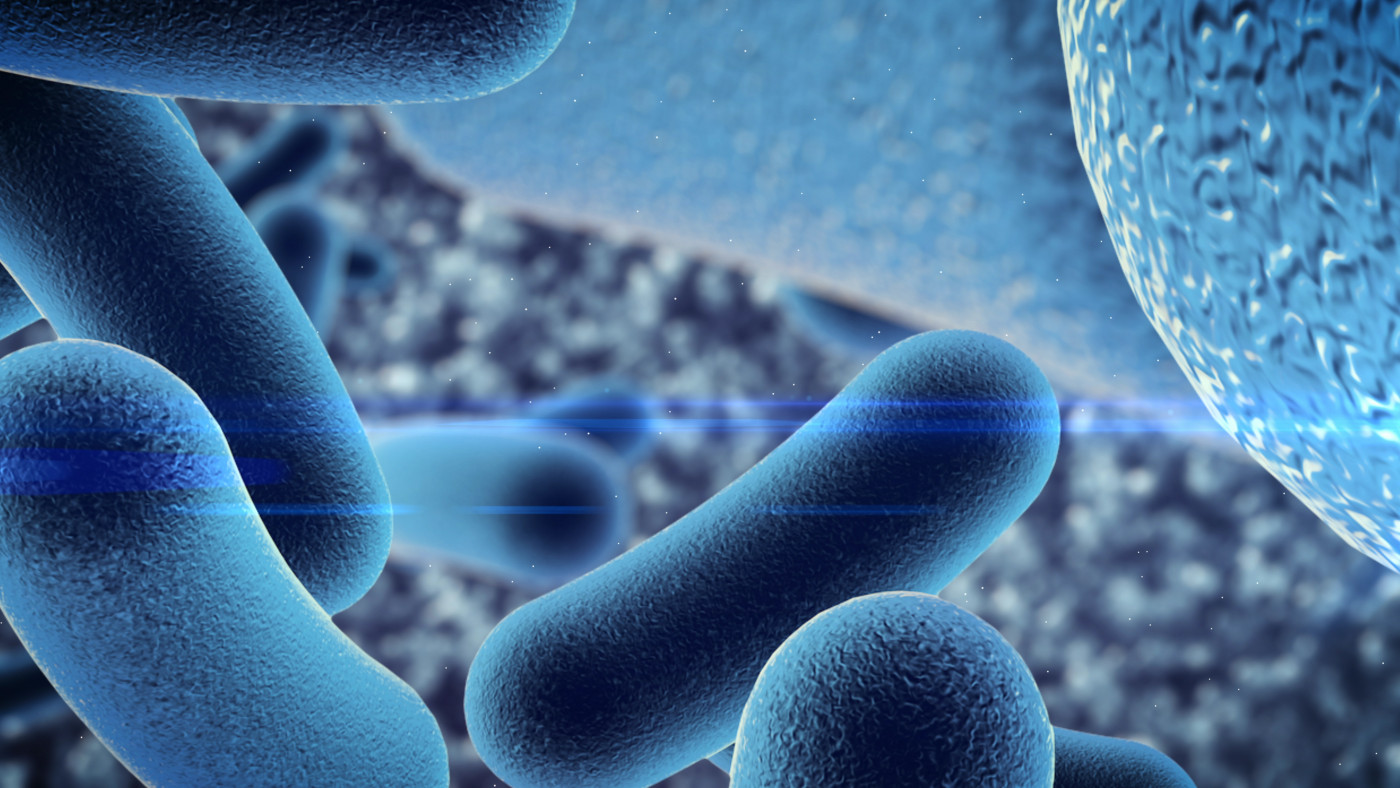
Pseudomonas aeruginosa, a bacteria that commonly causes serious lung infections in people with cystic fibrosis (CF), reacts to other dangerous bacteria in ways that could be exploited to develop new antimicrobial treatments, early research has found.
When Staphylococcus aureus is present, P. aeruginosa starts moving faster toward that bacteria, invading and destroying its colonies. These finding offer insights into how disease-causing bacteria compete with each other, which could help identify strategies to harness these interactions, paving the way for new antimicrobial strategies, the researchers said.
The study, “Interspecies interactions induce exploratory motility in Pseudomonas aeruginosa,” was published in the journal eLife.
Bacteria, fungi, and even some viruses can sense and communicate with each other, with important consequences for their survival and proliferation.
Communication between bacteria can change how they behave and impact disease progression. For example, airway infections with both S. aureus and P. aeruginosa — two bacteria prevalent in chronic infections — have been linked with poorer outcomes in CF patients, in terms of worse lung function and shorter lifespan.
To determine in more detail how these two important bacteria interact, a microbiology and immunology professor at the University of Iowa and her colleagues used a special system in the lab to grow both bacteria together. The team, led by Dominique Limoli, PhD, then tracked each bacteria’s movements over time under the microscope.
“One strategy to improve outcomes for people with cystic fibrosis carrying multiple infections is to block harmful interspecies interactions before they begin,” Limoli said in a press release.
“We designed a system to visualise the early interactions between two microbes that cause infections in people with cystic fibrosis to follow their behaviour over time,” she said.
By imaging the two bacteria, researchers saw that when P. aeruginosa is alone it grows into bacterial groups that look like “rafts” under a microscope. But in the presence of S. aureus, P. aeruginosa bacteria transition from a collective to single cells known as “exploratory.” These explorer bacteria moved quickly in the direction of S. aureus colonies. Once they got there, P. aeruginosa bacteria invaded the S. aureus colonies, and end up dismantling them.
Studying this observation in more detail, the researchers found that P. aeruginosa adopts this behavior because it senses and responds to substances released by S. aureus into the environment, triggering mobility alterations.
The team proved this by putting P. aeruginosa in contact with liquid in which S. aureus had been growing. This media made P. aeruginosa move much faster in petri dishes in the lab.
To see if this would hold true for other types of bacteria found in the airways of CF patients, the team repeated these experiments. They used three other bacteria taken from CF clinical isolates — namely Haemophilus influenzae, Burkholderia cepacia, and Achromobacter xylosoxidans. One of them, B. cepacia also enhanced the movement of P. aeruginosa.
The researchers also looked at a broader group of bacteria not associated with cystic fibrosis, including salmonella, Escherichia coli and Bacillus subtilis. They found all significantly increased the mobility of P. aeruginosa.
“By acquiring a fundamental understanding of how bacteria sense and respond to life with each other, we move closer to learning how to rationally manipulate these behaviors during infection and in the environment,” Limoli said.
“For cystic fibrosis patients, this may mean preventing P. aeruginosa and S. aureus physical interactions. In other instances, we might bring together bacterial species that synergize to produce a beneficial compound,” Limoli added.
The team believes that “identifying strategies to harness these interactions may open avenues for new antimicrobial strategies.”