Lung function in CF seen to worsen faster after Pseudomonas infection
Link between bacteria and worse function strongest in adolescence
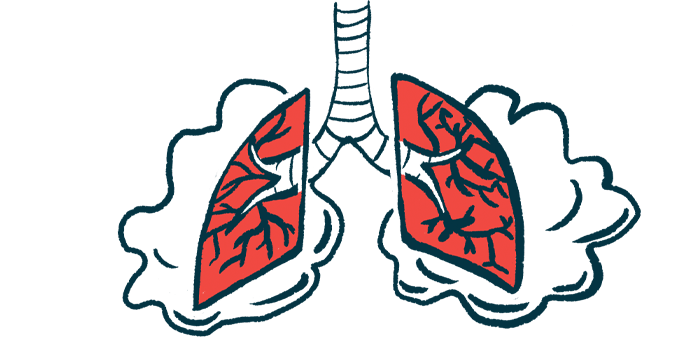
Among children with cystic fibrosis (CF), lung function was seen to worsen faster following a bacterial infection with Pseudomonas aeruginosa, especially if the infection became chronic or ongoing, a new study reports.
The link between the bacterium — commonly known as Pseudomonas or P. aeruginosa — and a worse decline in lung function was strongest during early adolescence.
“As lung function … is a strong predictor of survival, understanding and addressing risk factors for lung function decline is critical to improving long-term outcomes in CF,” the researchers wrote, highlighting a need for treatments to prevent infections, especially during the teenage and preteen years.
“Our findings suggest that measures to prevent chronic infection, particularly during the high-risk period of early adolescence, could mitigate [lung function] decline and improve survival,” the team wrote.
The study, “Association of Pseudomonas aeruginosa infection stage with lung function trajectory in children with cystic fibrosis,” was published in the Journal of Cystic Fibrosis. It was funded by the Cystic Fibrosis Foundation.
Pseudomonas infections in CF occur in over 60% of patients by age 6
CF is characterized by thick mucus in the lungs, which sets the stage for inflammation and frequent bacterial infections that damage lung tissue. In most people with CF, lung function gradually worsens over time as the lungs become progressively more damaged. However, the rate of lung function decline varies from person to person.
Pseudomonas is a key bacterial agent in CF lung infections. Due to the well-established risks associated with this bacteria, people with CF are usually monitored for Pseudomonas regularly. If it’s detected, patients are typically given antibiotics with the aim of wiping out the infection. This is often successful, though many patients develop chronic infections that are difficult or impossible to completely eliminate.
In this study, researchers analyzed how Pseudomonas infection affects the rate of lung function decline among children with CF. To do so, they turned to data from the Early Pseudomonas Infection Control (EPIC) observational study (NCT00676169). From 2004 to 2006, this observational study enrolled children with CF, ages 12 and younger, who did not have a documented Pseudomonas infection, at dozens of centers in the U.S.
The analysis covered data for 1,264 CF patients with at least two measures of forced expiratory volume in one second (FEV1) recorded between ages 6 and 21. FEV1 is a common measure of lung function based on how much air someone can forcibly blow out in a second. It’s not done before age 6 in the U.S. CF Registry.
By age 6 when the first FEV1 measure was recorded, 63% of the patients had tested positive for Pseudomonas at least once. Over the years of follow-up, the number of patients who’d never had an infection decreased, while the number of those developing chronic infections increased.
Statistical models, which accounted for other clinical factors and treatment patterns, showed that the rate of decline in FEV1 was significantly slower in patients who had never had a Pseudomonas infection compared with those who’d ever had such an infection.
The rate of decline in FEV1 was fastest among patients who had chronic Pseudomonas infections. The researchers noted that there is not currently a standardized definition for when an infection can be deemed chronic, but results using several different proposed definitions all yielded broadly similar results.
These results overall are in line with other research that’s shown a connection between Pseudomonas infections and faster lung function decline in CF — though the scientists highlighted that this study had a much longer follow-up than most prior research.
Highest risk seen in CF teens and preteens with Pseudomonas
Models suggested that the rate of lung function decline tended to be fastest during early adolescence, around ages 12 to 14. The association between Pseudomonas infection and faster FEV1 decline was strongest around this age.
“We do not have a clear explanation for this finding of maximum decline in FEV1, especially with chronic [Pseudomonas infection], in early adolescence,” the researchers wrote.
The team speculated that, because this age range is usually a period of intense airway growth — a “critical window” — as the body enters puberty, it’s possible that infections or inflammation in the lungs could have more pronounced and harmful effects because they could interfere with lung health.
However, the researchers stressed that, from these data alone, it’s impossible to say whether Pseudomonas directly causes faster FEV1 decline. Another notable limitation of this study is that it was done prior to the availability of CFTR modulators, a recent class of medications that can boost the functionality of the disease-causing mutated protein in people with specific types of mutations.
“The association between [Pseudomonas] infection and disease progression in the [CFTR modulator] era may differ from that in our cohort,” the researchers wrote. “For now, our findings suggest that further measures–potentially in addition to [CFTR modulators]–to prevent chronic infection could mitigate FEV1 decline and improve survival.”